To understand what a herniated disc is, you must first understand what a "disc" is. Intervertebral discs are the soft disc-shaped connective tissue cushions between the individual bones of the spine. These discs' act like shock absorbers and minimize the impact of movement on the vertebrae. The unique architecture of the intervertebral discs allows them to function even under constant pressure from the vertebrae. An intervertebral disc is shaped somewhat like a jelly doughnut. It has a softer inner part called the ‘nucleus' that is encapsulated in a tougher rubbery exterior called the ‘annulus' (1).
A herniated disc results when there is an abnormal rupture in the rubbery exterior part or the annulus. The break causes the softer part of the disc to push through or ‘herniate.' As the inner part of the intervertebral disc literally ‘slips' from its original place, a herniated disc is also known as a ‘slipped disc.'
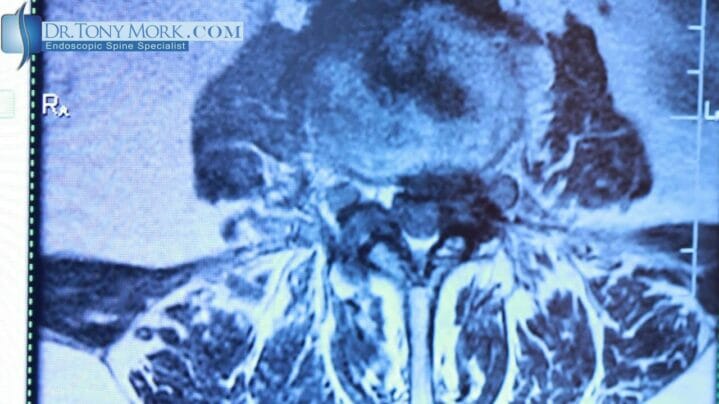
Although disc herniation can occur at any level, the most common location is the lumber region of the spine or the lower back. The lumbar part of the spine is consistently absorbing an extraordinary amount of pressure, and hence it is more susceptible for herniation.
A herniated disc can cause severe irritation to the adjacent nerves resulting in pain, numbness and occasionally weakness (2). The weakness may be observed in either arms and legs, depending on the nerve affected. However, not all patients suffering from a herniated disk will experience all the symptoms.
Herniated Disc Causes
This is where the spinal disc’s nucleus pushes backwards and expands the edge of the annulus. Herniation basically comes in three forms: a non-contained herniation, a sequestered fragment herniation and a contained herniation. In a contained herniation, the nucleus’s center tends to ooze out of the spinal disc via an annular tear. There is basically a rupture inside the annulus which moves out but gets contained by the longitudinal ligament.
This, in turn, leads to chronic back pain. In a sequestered fragment herniation, the nucleus extends beyond the posture longitudinal ligament, and it also spreads beyond the annular tear. Here, a portion of the nucleus completely loses continuity with all the other portions of the nucleus. With a non-contained herniation, the nucleus of the spinal disc extends beyond the annular tear. It also moves outside the posture longitudinal ligament, which is incapable of containing it.
So with that being said, herniated discs can occur naturally and there can be a number of causes, as any activity would irritate the nerves in the instance of a herniated disc. The most common cause of herniation is the natural wear and tear of the spine and simply just the natural aging process. But there are situations where an injury causes the bulging disc. It's common in weightlifters, with the most typical being injuries from a deadlift exercise as one example. A severe car accident or trauma could cause a disc to herniate as well.
Herniated Disc Symptoms
A herniated disc has many hallmark symptoms. However, not all people suffering from a slipped disc experience every symptom. Some of the most common symptoms include the following.
- Intense pain in arms or legs. Pain is one of the most common symptoms of a herniated disc.
- If herniation occurs in the lower back region, the pain is most intense in the buttocks, calves, and thighs.
- If the herniation occurs in the neck area, the pain is most severe in the shoulders and arms. Any position or activity that leads to compression of the slipped disc can cause pain to shoot through the extremities.
- Numbness and tingling: Some people may also experience numbness and tingling due to a herniated disc. It may or may not accompany pain.
- Weakness: A herniated disc can also cause muscular weakness depending on the nerves affected.
Herniated Disc Treatment Options
The treatment of a herniated disc depends on the magnitude of the herniation and the symptoms presented by the patient. While some patients may exhibit chronic symptoms, some others may be fairly asymptomatic. The course of action to treat a herniated disc can follow a more conservative (non-invasive) approach or a surgical approach. Dr. Mork utilizes Endoscopic Spine Surgery, as a herniated disc treatment and has successfully relieved many patients of their back pain with over 8,000 surgeries performed.
Pharmaceutical drugs
Several pharmaceutical drugs are used to treat a prolapsed disc. Although these drugs don't revert the damage, they offer a temporary symptomatic relief. The drugs used to fall in various categories that include the following.
Non-prescription pain medications
Many over the counter Non-Steroidal Anti-Inflammatory Drugs (NSAIDS) are routinely prescribed to the patients suffering from a herniated disc (3). These drugs are the most efficient if the pain is mild to moderate. Medicines in this category include Ibuprofen, Naproxen, etc.
Prescription pain medications
The doctor may prescribe stronger pain medications including narcotics if the NSAIDS are ineffective. Drugs such as Percocet and OxyContin may be prescribed for a short duration to deal with chronic pain. These more potent pain medications have side effects of their own and should not be used for an extended time. They are notoriously habit-forming and should be utilized with caution.
Anti-seizure medications
These drugs are usually used to treat seizures. However, in the case of a severe nerve pain associated with a herniated disc, these drugs can act as pain relievers. These medicines calm the aggravated nerve and reduce the pain significantly. However, as with narcotics, these drugs have their side effects and should not be taken for a prolonged time.
Muscle relaxants
A herniated disc can cause muscle spasms as a secondary indication. Muscle relaxants can relieve these spasms and help in mobility and pain. These drugs may cause drowsiness and sedation, hence, should be used with caution.
Steroid injections
Disc herniation can cause severe inflammation in the nerves and adjoining area. The inflammation, in turn, causes pain. Steroids such as cortisone can suppress inflammation. Direct injections of cortisone to the area adjoining the prolapsed disc may relieve pain and inflammation. Oral steroids are also prescribed in some cases to control inflammation further.
Physical Therapy
Physical therapy can help alleviate symptoms of a herniated disc. Various methods used in physical therapy can offer immediate as well as long-term benefits in slipped disc patients (4). Some of the techniques utilized in the treatment of herniated disc include the following.
Deep tissue massage
This technique relieves the spasms and tensions in the deep muscles associated with herniated disc. Deep tissue massage can restore muscle mobility and can also offer relief from deep muscular pain due to a slipped disc.
Heat and Cold Therapy
Both heat and cold therapies can provide benefits to a patient suffering from a herniated disc. Heat therapy increases blood circulation in the affected area causing the flushing out of pain and spasm causing substances such as lactic acid. On the other hand, cold therapy restricts the blood flow to the injured disc and hence can reduce inflammation. A physical therapist may use both hot and cold therapy alternately to achieve the desired relief.
Transcutaneous Electrical Nerve Stimulation (TENS)
The TENS procedure utilizes electric impulses to stimulate the muscle tissue. It can relieve spasms and pains when other methods fail. TENS is perfectly safe and uses only a small amount of electric current to stimulate the muscles.
Traction
Traction is yet another standard physical therapy practice that is used in the treatment of herniated disc. The logic is to pull the bones apart by applying weight so that the prolapsed disc can slip back in its place.
Physical exercises
Physical exercises to strengthen the core, improve flexibility and strengthen muscles can help patients with herniated disc. These activities contribute to decreasing the pressure on the herniated disc thereby alleviating symptoms such as pain and weakness.
Surgery
In some patients, herniated disc surgery is the only option to get a permanent relief. However, only a small number of patients suffering from herniated disc must undergo surgery.
The surgery involves the removal of the portion of the disc that has herniated (5). However, in some cases, the entire disc needs to be removed. In such situations, the surgeon may either fuse the two adjacent vertebrae or insert an artificial disc between them. The fusion of the vertebrae with spinal wire restores the stability of the spinal column. However, some mobility is lost. Implantation of an artificial disc costs more and is rarely performed.
Alternative treatments
Several alternative medicine disciplines can offer some help to patients with a herniated disc. Spinal arrangement by a chiropractor can contribute to alleviating the pain and muscle spasms. Some people also find acupuncture to be helpful in the treatment of pain associated with a herniated disc.
References:
(1) Raj, P. P. (2008). Intervertebral disc: anatomy-physiology-pathophysiology-treatment. Pain Practice: the Official Journal of World Institute of Pain, 8(1), 18–44. http://doi.org/10.1111/j.1533-2500.2007.00171.x
(2) Chapter-01 Back Pain, Sciatica and Herniated Lumbar Intervertebral Disc Historical Anecdote. (2014). Chapter-01 Back Pain, Sciatica and Herniated Lumbar Intervertebral Disc Historical Anecdote (pp. 1–3). http://doi.org/10.5005/jp/books/12000_1
(3) Sonntag, V. K. H. (2010). Treatment of the Herniated Lumbar Disc: Persistent Problem. World Neurosurgery, 74(6), 574–575. http://doi.org/10.1016/j.wneu.2010.08.006
(4) https://www.spineuniverse.com/conditions/herniated-disc/physical-therapy-herniated-discs
(5) Ramadan, A., Hassan, A., & Khalaf, N. (1997). Indications for surgery for herniated lumbar disc. Clinical Neurology and Neurosurgery, 99, S163. http://doi.org/10.1016/S0303-8467(97)82023-9