What is Herniated Disc surgery?
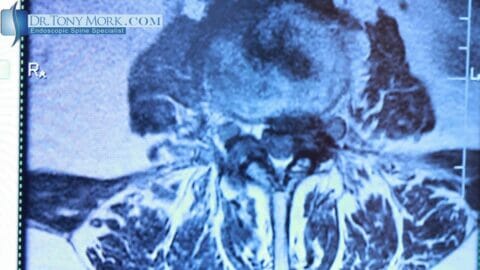
Herniated disc surgery is performed for persistent pain, weakness or numbness. The pain or weakness must correspond to the nerve that is being pinched or compressed by the disc herniation and that is why a good history and examination is necessary to correlate these findings. Sometimes the disc can be herniated to the side opposite of your symptoms. This happens occasionally and I usually perform surgery on the side of the pain as long as the symptoms match the level of the disc herniation.
Category: Disc Herniation
Topics on herniated discs are covered in this section of the blog. Bulging discs and protrusions will be discussed as well. Everything from what a bulging or herniated disc is, to symptoms, causes, and treatment options.
What is Disc Herniation? Symptoms, Causes and Treatment Options
To understand what a herniated disc is, you must first understand what a “disc” is. Intervertebral discs are…
Deadlift Back Pain: You Should Read This If You Lift Weights
Deadlift Back Pain I get to hear about back pain every day as an endoscopic spine surgeon. Back…
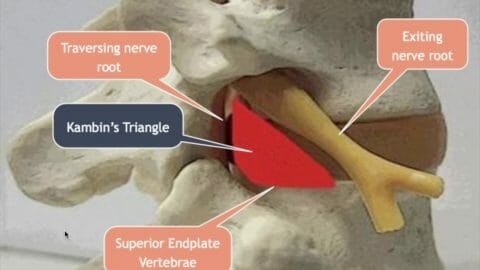
Lumbar Transforaminal Approach for Herniated Disc
Today, everybody talks about doing minimally invasive spine surgery, but that’s about the extent of it. There really…
A Few Tips to Strengthen Your Lower Back To Prevent a Herniated Disc
Other times called a ruptured or slipped disk, a herniated disc in most cases occurs in the lower…
Bulging Disc and Herniated Discs | Symptoms, Causes and Treatments
You may have had a medical exam that revealed an underlying health problem. The physician explained that you…
Is Herniated Disc Surgery The Right Approach?
Is surgery right for you? Apart from being an author and public speaker, I’m also an orthopedic…
Dr. Mork on Herniated Disc: Symptoms, Diagnosis, AND Treatment
Most of us might think that pain within our backs is just a simple matter that we can…