Today, everybody talks about doing minimally invasive spine surgery, but that’s about the extent of it. There really isn’t a definition and worse yet, some people imply that fusions are minimally invasive. It’s true that a fusion can be performed with minimally invasive techniques, but it’s an irreversible procedure that cannot be undone.
The chances are good that you need spine surgery, if you are looking at this. Most likely you have a disc herniation or foraminal stenosis that is causing you some pain, numbness or weakness and you want to relieve this pain. The question is, how to approach this problem to decompress or remove it.
In many ways, the spine can be likened to a series of bony tubes or canals that are joined from the skull to the tailbone.
The purpose of these canals is to provide safe passage of the spinal cord and nerves that travel from your brain to your hands and feet. The concept of safe passage sounds very comforting, but what if there is a problem inside of the hollow tubes, like a disc herniation? Now we have a problem that we need to access to relieve your pain.
The Door Way to Safely Get to a Herniated Disc
Now we are looking for a door or doorway to safely enter the spinal canal and remove the disc herniation. Ideally, we’d like a doorway that already exists and is safe to access. Safe means that we are going to be able to see and access the disc herniation without injuring any nerves or causing any significant bleeding. Does such a doorway exist?
Yes it does, but it’s a small doorway and it’s triangular.
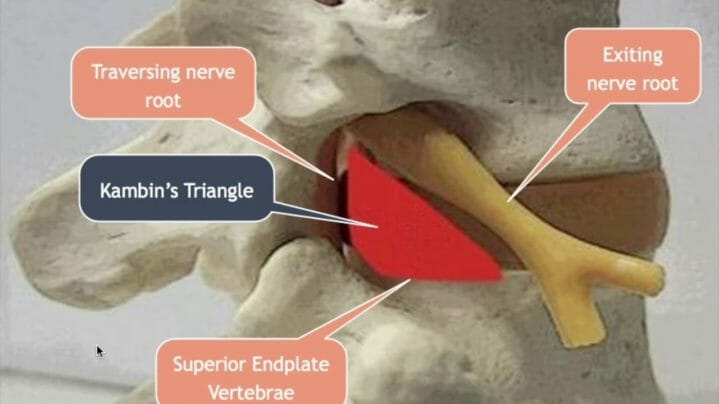
Dr. Kambin originally described this small doorway decades ago and it is called Kambin’s Triangle, which is really the Transforaminal Approach. He described a naturally existing, but small doorway to approach the disc in the lumbar spine. This triangular doorway is bordered on three sides by the exiting nerve root, “spinal cord”, and endplate of the vertebrae. This triangle is the safe way to the disc herniation.
Doesn’t this sounds great?
A safe way to the disc herniation that doesn’t require any bone removal, like a laminectomy or laminotomy does. So why doesn’t everybody use this approach for disc herniations? The reason is that the instruments have to be very small and have to be pretty long because of the angle of approach needed.
In addition, there needs to be a light source that can reach that far as well as a way to retract the tissues so you can see the herniated disc. Is such an instrument available?
Yes!
The Transforaminal Endoscope
Although the dimensions are a little different, it is basically the same instrument used in knee and shoulder surgery. The arthroscope essentially revolutionized knee and shoulder surgery back in the 80’s and other specialties have followed, like general surgery and gynecology. I don’t know of any patient or doctor using endoscopic techniques that ever looks back and says, “I wish we could make the incision larger again”. The endoscope takes the term “minimally invasive” to a whole new level.
So let’s review how we can approach a herniated disc endoscopically. We’ve talked about a small, naturally occurring triangular doorway into the spine called Kambin’s triangle. This doorway is triangular and bordered by the exiting nerve root, “spinal cord” and vertebrae. It can be accessed and entered safely with a transforaminal approach using a transforaminal endoscope.
The Benefits of the Transforaminal Approach for a Herniated Disc
There are two very special benefits when using the endoscope for the transforaminal approach.
- The first is an enclosed water environment. This means no air will contact the surgical site, and the tissues can’t dry out because there is no contact with the air. I also think that no air contact means less formation of scar tissue. This is a hermetically sealed system; there is no way for air or germs to enter the surgical site from the room. A continuous flow of water will wash all debris out and maintain crystal clear vision during surgery.
- The second benefit is related to the way the tissues are retracted to see the herniated disc. In any environment where the surgical site is in contact with room air, there is no positive pressure to keep tissues retracted to see the operative field. This means that the walls of the metal tube must exert pressure on the soft tissues to retract them.
In the case of a hermetically sealed endoscope, water is constantly pumped into the operative field under pressure, so the positive pressure created at the tip of the scope creates the operative field. In other words, it is hydraulic pressure that retracts the tissues, not a metal tube. Think of a balloon on the end of a straw.
Most lumbar disc herniations can be removed with this approach, but not all. We will talk about another “doorway” into the spine called the Interlaminar Approach for those disc herniations that cannot be removed with the transforaminal approach.
Let’s look at three ideal situations to use the transforaminal approach.
- One is the para-central disc herniation. The endoscope is placed through the foraminal canal and directed to the disc herniation on the right or left side. The herniation cannot migrate too high or low from the intervertebral disc space or it can’t be reached.
- Two is the foraminal disc herniation in the foraminal canal. This is the ideal situation for the transforaminal approach to minimize surgical exposure. The scope is small enough to enter the foraminal canal and remove the foraminal disc herniation.
- Three is the situation where the foraminal canal is too tight and the exiting nerve root gets squeezed. This is called foraminal stenosis and is caused by over growth of bone, disc or facet joint capsule into the foraminal canal.

In the case of the 7 mm transforaminal endoscope, it is the small size of the scope that allows the surgeon to get to places that are otherwise not possible. The small scope uses an incision of about 3/8”. The typical tube size used for “minimally invasive” spine surgery is 16 mm and larger, not a 7 mm like the transforaminal scope.
So size does matter. It matters in terms of what you can access and where you can go, not to mention minimizing collateral soft tissue damage. The trasnsforaminal approach is indispensable to remove certain disc herniation’s and represents the ultimate in minimally invasive spine surgery with a diameter of 7 mm.