Stenosis is a Greek term which means “narrowing”. Imagine a narrowing in a water way, like a river,…
Category: Spinal Stenosis
What is Spinal Stenosis? | Causes, Symptoms & Treatment Options
Spinal stenosis is a common condition that occurs when the space around the nerves or spinal cord narrows.…
Worried About Lumbar Stenosis?
Find Out Who’s Worried About Lumbar Stenosis and Why You Should Listen to Them When surgery is necessary,…
The Ins and Outs of Cervical Spinal Stenosis
The spinal cord comprises a column of nerve tissues that are safeguarded by a canal which runs through…
Controlling Lumbar Stenosis Without Surgery or Medication
The spine is one of the most important components of the human body. The whole system of bone,…
What is Spinal Stenosis?
What is Spinal Stenosis? Any individual who suffers from back, leg, or arm pain may find that they…
Stenosis In The Neck | Cervical Spinal Stenosis
It’s not at all uncommon for people to learn about their spinal stenosis from x-ray or MRI…
Disc Herniation and Spinal Stenosis
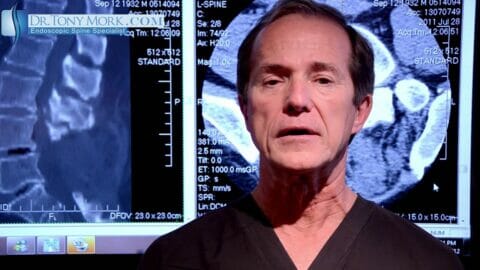
In this video Dr. Tony Mork describes a way to treat the combination painful stenosis with a disc…