Back pain is actually really common. A question presented to me recently was “What is the prevalence of…
Category: Back Pain Blog
Back Pain Causes | A Brief Overview
So What are the Causes of Back Pain? There are many causes of back pain and we…
What Is Lumbar Spinal Stenosis?
Stenosis is a Greek term which means “narrowing”. Imagine a narrowing in a water way, like a river,…
What is Spinal Stenosis? | Causes, Symptoms & Treatment Options
Spinal stenosis is a common condition that occurs when the space around the nerves or spinal cord narrows.…
Everything You Need to Know About An Annular Tear
Annular tears are probably the most misdiagnosed condition when it comes to lower back pain. Most adults suffer…
Herniated Disc Surgery
What is Herniated Disc surgery?
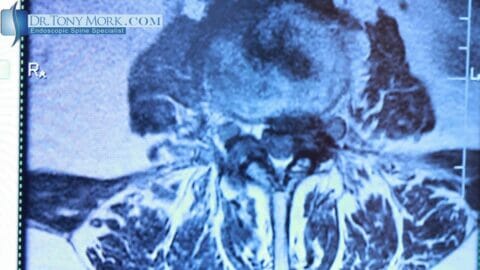
Herniated disc surgery is performed for persistent pain, weakness or numbness. The pain or weakness must correspond to the nerve that is being pinched or compressed by the disc herniation and that is why a good history and examination is necessary to correlate these findings. Sometimes the disc can be herniated to the side opposite of your symptoms. This happens occasionally and I usually perform surgery on the side of the pain as long as the symptoms match the level of the disc herniation.
Cervical Foraminal Stenosis Symptoms
If you have pain in the neck that radiates to the shoulder (usually the back or top of…
Cervical Foraminal Stenosis Treatments
There are many people with pain that radiates into the shoulder, arm or hand who get an MRI…
What is Disc Herniation? Symptoms, Causes and Treatment Options
To understand what a herniated disc is, you must first understand what a “disc” is. Intervertebral discs are…
Cervical Foraminal Stenosis Diagnosis
How is Cervical Foraminal Stenosis Diagnosed? The diagnosis of cervical foraminal stenosis comes after the onset of symptoms,…
Deadlift Back Pain: You Should Read This If You Lift Weights
Deadlift Back Pain I get to hear about back pain every day as an endoscopic spine surgeon. Back…
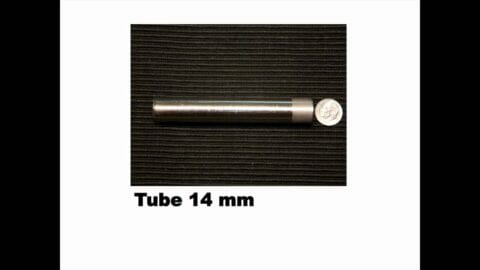
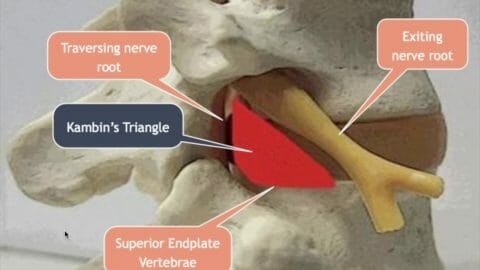
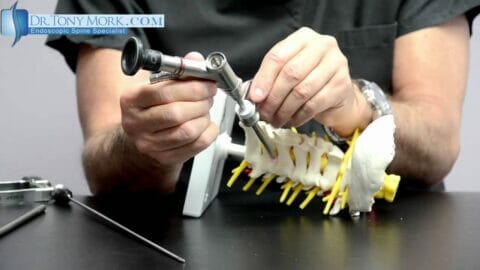
Lumbar Transforaminal Approach for Herniated Disc
Today, everybody talks about doing minimally invasive spine surgery, but that’s about the extent of it. There really…
Lumbar Foraminal Stenosis Problems And Treatment Part 2
Hi, I am Dr. Tony Mork, author, speaker, endoscopic spine specialist. Today I am going to do part…
The Causes of Cervical Foraminal Stenosis
We have discussed the symptoms or things that you feel in your neck, shoulders, arms and hands when…
Worried About Lumbar Stenosis?
Find Out Who’s Worried About Lumbar Stenosis and Why You Should Listen to Them When surgery is necessary,…
Lumbar Foraminal Stenosis Problems And Treatment Part 1
Hi, I am Dr. Tony Mork, author, speaker, inventor and endoscopic spine specialist. Today I would like to…
Pinched Nerve Double Crush Syndrome
Last year I saw a gentleman with complaints of pain and numbness in the neck, shoulder, arm and…
What Mimics a Pinched Nerve?
In Pinched Nerve, we talked about what happens to a nerve that gets squeezed or compressed between 2…
The Ins and Outs of Cervical Spinal Stenosis
The spinal cord comprises a column of nerve tissues that are safeguarded by a canal which runs through…
Controlling Lumbar Stenosis Without Surgery or Medication
The spine is one of the most important components of the human body. The whole system of bone,…