The term minimally invasive gets thrown around by doctors a lot. The "invasiveness" of a procedure typically is measured by the size of the incision, or amount of tissue damaged in the process.
What usually is not associated with the terms minimally invasive, is the impact the procedure has on you.
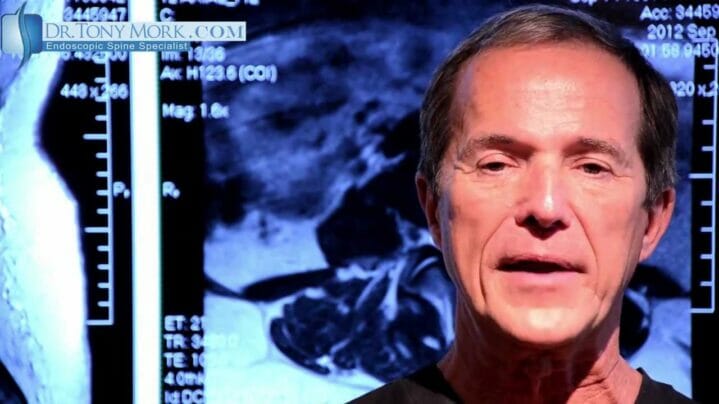
In my video I talk about a patient who suffered from post-operative pain and continued problems, after going what was described to him as a minimally invasive surgery. On the surface, the scar would have you think that the surgery was a small, non-invasive procedure. After reviewing his MRI scans however, I could immediately tell what was going on.
Minimally Invasive Does Not Always Mean Minimally Impacting
The patient had undergone a fusion across multiple disc spaces, with multiple facet screws immobilizing that section of the spine. Take a look at the video above to see his scans and how much hardware was actually installed.
Minimally Invasive AND Minimally Impacting
I always describe my procedures as endoscopic as well as minimally invasive to avoid any miscommunication about what is being performed on my patients. My philosophy is to NOT fuse the spine, and use NO hardware.
Through new techniques and tools that I have helped invent and design, we can now perform endoscopic spine surgery through an incision smaller than a nickel. Without all the extra hardware involved, you can be healed and back on your feet within a week. In fact, most of our patients usually feel immediate pain relief.
The Take Away From This
Always make sure that when you are referred for a minimally invasive procedure, you know exactly what the procedure entails. Fusions often are not minimally invasive, no matter how you dress them up. They have longer recovery times and require the use of larger tools and equipment.
As always, we offer phone consultations to anyone that would like to talk about their pain or review their previous MRI scans.